Transforming CQC Feedback into Excellence: Key Insights from our Latest CQC Webinar
14 May 2024
Tags:
 CQC Webinar Recap: Turning Feedback into Excellence with Radar Healthcare
CQC Webinar Recap: Turning Feedback into Excellence with Radar Healthcare
Did you miss part 1 of our CQC webinar, “Transforming Feedback into Excellence: Evidencing Outstanding Care Quality for CQC Success with Radar Healthcare”? Here’s a recap of the insightful discussions and key takeaways from our expert panel.
The Care Quality Commission (CQC) plays a pivotal role in ensuring that health and social care providers in the UK meet the necessary standards to deliver safe and effective care. With the new single assessment rolled out in the UK, organisations need to consider several things to achieve CQC excellence; including, how to evidence compliance and excellence, how to gather feedback and drive learning, and how to properly support and prepare your team for inspections. These were central themes of our latest webinar held on Thursday, 9th May 2024.
Meet our expert panel
-
Simon Qasir
Chief Revenue Officer at Radar Healthcare
-
Antony Hall
Director of Regulation at HC-One
-
Mark Fewster
Chief Product Officer at Radar Healthcare
Watch our Exclusive CQC Webinar
Led by Simon Qasir, Chief Revenue Officer and Board Director at Radar Healthcare, alongside Antony Hall, Director of Regulation at HC-One and former CQC inspector. Completing the panel was Mark Fewster, Chief Product Officer at Radar Healthcare, and Home Manager at Admirals Reach (Chelmsford), the expert panel sheds light on the new CQC framework, the impact this has on health and social care organisations, and best practice to achieving CQC excellence.
Topics covered:
📚 Understand the CQC’s new framework
🔍 How to evidence compliance and excellence
🏆 How to prepare your team for CQC interactions
💡 Real-life Success Stories from HC-One
Understanding the CQC Changes and the Impact on Your Organisation
As we know, the CQC Introduced significant updates that are changing the way they assess health and social care organisations in the UK. These modifications aim to push organisations towards a higher standard of care through enhanced accountability, transparency, and patient-centered practices.
At the heart of these changes is a shift in how the CQC evaluates organisations. First and foremost, the shift to a single assessment framework means that all organisations and services from Care Homes and NHS Services to Home Care, GPs, and more will be assessed using the same criteria.

Shifting Priorities: The Growing Emphasis on Feedback and Evidence in Care Provision
The focus has broadened from not just what care providers do, but how effectively they are doing it, particularly in responding to and evidencing feedback and incidents. Out of the six evidence categories three of them are centered all around experience and feedback, making feedback crucial to achieving a Good or Outstanding rating. This evolution means that organisations must now ensure they have effective systems and processes in place for gathering, analysing, and acting on feedback from all stakeholders, including patients, families, and staff.
Additionally, the CQC’s updated framework places a stronger emphasis on evidence. Organisations are expected to document and evidence their practices, improvements, and responses to incidents comprehensively. This evidentiary requirement underlines the importance of robust document management systems and transparent operational processes.

“Throughout all the evidence categories there’s a very significant word that keeps reoccurring – learning. Within the new CQC framework you’ll find that they have put a real emphasis on being a learning organisation. The first quality statement focuses on cultivating a culture of learning. Under well led, emphasis is placed on capturing and leveraging lessons from both successes and failures to drive sustainable improvement. I think that gives us some great opportunities to demonstrate how we can learn as organisations, which has been the whole emphasis particularly in the health sector and more recently in social care for the last couple of years.”

Strategies for Documenting and Evidencing CQC Requirements
Navigating the complexities of CQC compliance necessitates a methodical approach to documentation and evidence management. Our recent webinar shed light on practical strategies that organisations can adopt to streamline this process. A pivotal element discussed was the implementation of sophisticated document management systems, designed to efficiently store, manage, and retrieve documents, ensuring that evidence is readily accessible during CQC assessments.
Effective documentation begins with a comprehensive understanding of the CQC’s expectations. Organisations are encouraged to develop standardised procedures for recording feedback, incidents, and events. These procedures should be clear, concise, and consistently applied across the organisation to ensure that all relevant information is captured in a timely and accurate manner.

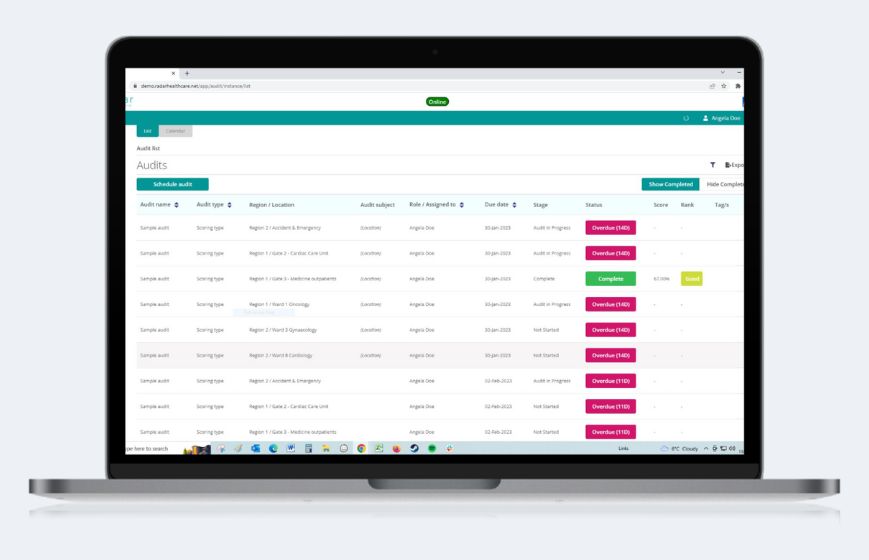
Incorporating technology plays a significant role in enhancing these processes. For example, digital feedback platforms can facilitate real-time gathering of patient and staff feedback, which can then be analysed to identify trends, areas for improvement, and opportunities to commend staff for excellent care.
Similarly, risk, quality, and compliance management and reporting software can help automate the reporting process, making it easier for staff to report incidents promptly and accurately, thereby enabling a quicker, more proactive response.
"Our focus is on enabling you to effortlessly access the evidence captured within the system. Beyond this, we're continuing to develop and add new features for capturing feedback and facilitating learning, encompassing inputs like complaints, compliments, and observations. Our aim is to provide you with the tools to effectively demonstrate the quality of your evidence to the inspectorate and then to further leverage this information for driving actionable change."

Empowering Staff and Elevating Care: Insights from Admirals Reach Care Home’s Quality Assurance Approach
Training and empowering staff is another critical strategy. Ensuring that all team members understand the importance of documentation and are equipped with the skills to effectively contribute to the process fosters a culture of accountability and continuous improvement. This approach not only aids in meeting CQC requirements but also in elevating the overall standard of care provided to patients.
The Registered Manager for Admirals Reach Care Home, 128 bed care home in Chelmsford shares their experience and strategy for gathering evidence from diverse stakeholders across their organisation:
“During the two-day inspection in January, we hosted a team of five inspectors, including a lead inspector, an associated inspector, and experts in various fields, such as nursing. They engaged with our staff, residents, and external professionals to assess key areas: feedback, experience, observation, communication, and learning. Understanding the shift in focus from paperwork to real-time interactions, we emphasised the importance of demonstrating quality care through firsthand experiences.
This involved continuous observation and evidencing, ensuring every aspect of resident care and choice provision was met. It is key to note that if you say you have implemented something or are making a positive impact, they will want to see evidence of that in various forms, including hearing from a resident, staff member, and so on. This is something our home did really well, and the feedback received underscored the importance of tangible evidence supporting our claims, highlighting the value of our approach to care.”
"As service managers, we were accustomed to the rigorous demands of the CQC inspection regime, with mechanisms in place to showcase evidence of quality care. However, the landscape shifted with the onset of COVID-19, prompting a transition to risk-based inspections. Recognizing the need to support our teams, we conducted workshops to familiarise them with the new framework and scoring mechanisms. It became evident that capturing feedback effectively was paramount, especially given the diverse sources—from formal surveys to ad hoc interactions. Emphasising the importance of observation, we provided practical tools and workbooks tailored to each service to facilitate evidence collection. This groundwork will be further enhanced with the introduction of the CQC dashboard from Radar Healthcare."

Fostering a Culture of Transparency, Accountability, and Readiness
Cultivating an organisational ethos where openness, responsibility, and preparedness are valued lies at the heart of excelling not only in CQC standards but in elevating care quality. A transparent culture encourages the free flow of feedback, where both staff and patients feel safe and understand how to voice concerns and suggestions. This open environment is crucial for identifying areas of improvement as well as celebrating achievements and highlighting organisational growth.
Preparation is equally important, enabling organisations and staff to respond swiftly and effectively to unforeseen challenges or feedback. This readiness is not just about having policies and procedures in place but ensuring that these guidelines are ingrained in the daily operations and the mindset of the staff. Regular training, in person sessions, and drills can help reinforce this preparedness, ensuring that when the time comes, the staff can respond with confidence and efficiency.
The Registered Manager for Admirals Reach Care Home, highlights their mechanisms for ensuring staff feel prepared and supported:
“As a company, we prioritise e-learning and specialised training, particularly focusing on security frameworks and infection prevention and control (IPC). It’s crucial that this training translates into practical application on the floor, where we actively engage our staff with specific questions and scenarios. This not only builds their confidence in interacting with inspectors but also ensures they are well-prepared to handle real-life situations. Through regular sessions and open communication, we foster a two-way exchange of knowledge, empowering our team to deliver high-quality care.”
Next Steps for CQC Excellence
To advance toward CQC excellence, organisations must undertake a dynamic and ongoing process of evaluation and improvement. Establishing a systematic approach for the regular review of processes, practices, and policies against the latest CQC standards and expectations is fundamental. Embracing technological solutions, like risk, quality, and compliance software, can streamline this review process, ensuring a seamless adaptation to regulatory changes and enhancing overall efficiency in documentation and evidence management.
Top three CQC takeaways 🚀
1️⃣ Engaging in continuous learning from both successes and challenges within and outside the organisation can foster an environment of perpetual growth and quality enhancement.
2️⃣ Implementing a structured feedback loop that includes analysis and action plans based on feedback from patients, families, and staff will be pivotal. This strategy not only supports compliance efforts but also elevates care and satisfaction for the that you support.
3️⃣ Preparing for CQC assessments should also involve regular staff training sessions focused on the updated criteria, to ensure everyone is confident, feels supported, and well-versed in what is required.
By prioritising quality and transparency throughout the organisation and with all stakeholders, you pave the way for no just meeting, but exceeding CQC standards. Achieving excellence requires a unified effort, utilising every available tool, resource, and feedback to continually elevate the standard of care provided.
“We recognise the challenges ahead, but I think organisations need to be optimistic about the opportunities they bring. The structured evidence categories focusing on observation, feedback, and experience enable us to showcase our dedication to delivering exceptional care. It's a shift from paperwork to prioritising the individual's care experience. Embracing this change and leveraging technology will ultimately lead to better health and care outcomes for everyone."

Sign up here Q&A from webinar
This is indeed a significant challenge we’re facing. CQC also struggles with this issue to ensure the voices of such individuals are heard. One approach is through visual aids and engaging with dementia communities to better understand their perspectives. Additionally, families play a crucial role in providing insights.
CQC has been preparing to address this challenge by emphasising observation. They assess interactions and changes in mood states to capture these individuals’ voices effectively. While observation serves as a primary method, alternative approaches or data collection methods can still integrate into our system to ensure comprehensive evidence aggregation.
There will be no cost associated with this. We anticipate that the dashboard will be accessible by the end of June 2024.
The observation aspect may take a bit longer as we refine the data capture process in collaboration with experts. Our approach to the evolution of these tools is dynamic, with adjustments made based on user feedback. While the dashboard’s appearance may change over time, the underlying principle remains consistent.
One of our primary goals when we implemented Radar Healthcare was to shift away from simply providing reports and data to our staff. Instead, we aimed to empower them with the information they need to make tangible improvements within their service. It’s about giving them access to meaningful information rather than inundating them with raw data. This approach fosters a sense of ownership and accountability among staff members, as they become the drivers of change within their respective services. Additionally, we recognised the importance of learning from incidents and events. To facilitate this, we’ve developed a learning dashboard that allows us to track and share key learnings across our organisation. By embracing a culture of shared learning, we can collectively work towards improving the quality of care across the entire sector.
Learn more about our partnership between HC-One and Radar Healthcare
The versatility of customisable dashboards in Radar Healthcare extends beyond specific care settings. You can tailor these dashboards to unique needs and preferences. This flexibility allows for the adaptation of templates to address specific interests or requirements. For instance, if there’s a need to modify views or designs, customers have the autonomy to configure dashboards accordingly. For example, you may be a provider with services across various regions like Scotland and Wales, so this flexibility allows you to ensure you are being attentive to meeting the distinct regulatory standards of each jurisdiction.
For more information on customisable dashboards take a look here