Care Quality Commission: The state of care report 2021/22
14 November 2022
Tags:
Last year the CQC (Care Quality Commission) highlighted the risks of unmet needs across all sectors, with a big emphasis on the ever-growing numbers of people who are unable to access excellent quality care.
They stated that: “our health and care system is in gridlock, which is clearly having a huge negative impact on people’s care experiences”.
With hospital waiting times and ambulance response times climbing, as well as other emergency services struggling, the risks are worsening. Staff shortages and growing battles to recruit and retain staff create a vicious cycle that is damaging both the health and social care industry.
Although the CQC’s report revealed that overall 75% of NHS acute core services and 83% of adult social care were rated as good or outstanding, the percentage of people satisfied with the NHS’s service has dropped (from 53% to 36%), and many care homes and homecare services have reached their capacity of being able to admit more residents.
In this blog, we will cover the main points made in the ‘Care Quality Commission: The state of care report 2021/2022’ and address how some of these concerns can be eased with the help of technology.
Read CQC: The state of care report
Access to care
People are still suffering from the backlash of COVID-19.
A significant reduction in services across the sector, particularly NHS dental and GP appointments, means that people are struggling to access the care they need and are placed on extremely long waiting lists.
Moreover, 37% of people aged 65 and over who are on a health waiting list, said they did not feel well supported, and out of this percentage, 41% said that their quality of life has decreased whilst waiting for the urgent care they need.
The same study revealed that around half a million people are waiting for an adult social care assessment, for care or a direct payment to begin, or for a review of their health and care.
Due to long waits and limited access to care, the number of people seeking mental health support has also increased, putting more strain on the NHS services.
The shortage of staff and services, combined with the backlash of the pandemic, has added to the ever-growing backlog of people in need. At the beginning of the year, 2.2 million hours (about 251 years) of homecare could not be delivered, leading to unmet and under-met needs and extreme workforce burnout for those trying to do the job of multiple workers.
Shockingly, where you live could impact how long you wait for care too. People living in the worst-performing areas could be waiting 4 months longer than those located in better-performing areas.
Overall, the study showed that around half a million people are waiting for an assessment, care, or review of their social care needs.
Listen to What The Health Tech: Working towards Mental Health Awareness
Inequalities
Sadly, inequality continues to spread through the health and social care sector. The CQC urges organisations to ensure that they are aware of the inequalities and prioritise making care equal, accessible, and inclusive to all, whilst maintaining elevated levels of care with each experience.
Research shows that people living in deprived areas were more likely to have long-term conditions, illnesses, and disabilities. This could be pinned down to the fact that they typically use or have access to fewer health services than the average person.
In addition, people with disabilities, especially those in deprived areas, reported having had more negative experiences with health organisations than those living without disabilities or in a less deprived area.
Services like dentists were reported to be used more by people living in higher-income households (65%), in comparison to those living in the most deprived areas (43%), due to the high costs of treatment and checkups.
Ethnic minority-led GP practices are more likely to care for populations with higher levels of socio-economic deprivation and poorer health. This then increases the issues around recruitment and funding.
Radar Healthcare recently contributed to a report from Public Policy Projects ‘The Digital Divide: reducing inequalities for better health’. This report discusses the steps which need to be taken to ensure the introduction of digital patient pathways are done in a way that benefits all our communities, especially those in need of support.
Concerns
The report covers how “health and social care staff across the country are working relentlessly to ensure people are kept safe”.
This is reflective of the CQC’s July 2022‘s statistics; 83% of adult social care services, 96% of GP practices, 75% of NHS acute core services, and 77% of all mental health care services were all rated as good or outstanding for their service and care.
However, the report does address some serious concerns, particularly around access to safe maternity and pregnancy-related care. Studies found that women from ethnic minority groups are at a higher risk during pregnancy and childbirth and are more likely to be re-admitted to the hospital after giving birth.
July 2022’s study shows that 6% of NHS services are inadequate and 32% need improvement.
In addition, despite many reviews and reports, inequalities in care for people with learning disabilities and mental health services are still prevalent.
Listen to What The Health Tech: Bridging the Gender the Gap
Workforce crisis
The workforce crisis has been hitting the headlines for a while now, and sadly it is still a huge problem across all health and social care services.
With the Care Sector already predominantly offering low-paid work, Care workers across the country are struggling to cope with the rising costs and looking for higher-income jobs. In addition, workforce burnout is a huge problem for health and social care. The lack of staff increases pressures and impacts workers’ mental well-being and forces workers to seek work elsewhere.
CQC’s report revealed that 87% of care home providers and 88% of home care providers, who admitted to the workforce crisis having a negative impact, said they were experiencing recruitment challenges – and are unable to admit new residents.
Nearly 40% of providers said that workforce pressures are impacting the quality of care delivered to residents. 57% of NHS staff said they are struggling to meet demands, deliver high-quality care and manage duties during their work hours.
Over 2022, Radar Healthcare has worked alongside Public Policy Projects to contribute to and create a number of industry-based reports. ‘The Social Care Workforce: Adverting a Crisis’ report discusses in depth the state of the workforce crisis.
New systems
This year, Integrated Care Systems (ICSs) were formally introduced, and integrated care boards were set out in legislation, for health and social care organisations to bridge the gap between the two.
The main challenge new systems face is ensuring that they prioritise patients, residents, and staff’s experiences and are inclusive to all.
“Understanding the health and care needs of local people is paramount for integrated care systems, and each one faces a different challenge in meeting those needs. Good leadership will be vital for local systems as they become established during challenging times for all services. All services working in a local health and social care system should be included in planning for healthier communities.”
Read CQC: The state of care report
Summary: how can technology help?
It is apparent that increased stability across the sector is needed. Relieving the pressures within social care will ultimately relieve pressure on the NHS, by reducing the need for emergency services and delayed discharges.
Many healthcare organisations are opting for digital support to help them to deliver higher-quality care and support their workforce day-to-day.
Four Seasons Health Care Group consolidated its three systems into one, saving them time and money, as well as making them more efficient.
The most important thing for us is that we are providing the best care possible, and Radar Healthcare helps us do just that.
Radar Healthcare’s risk, quality, and compliance software has been designed to support all health and social care organisations, big or small, to make a difference, now and in the future.
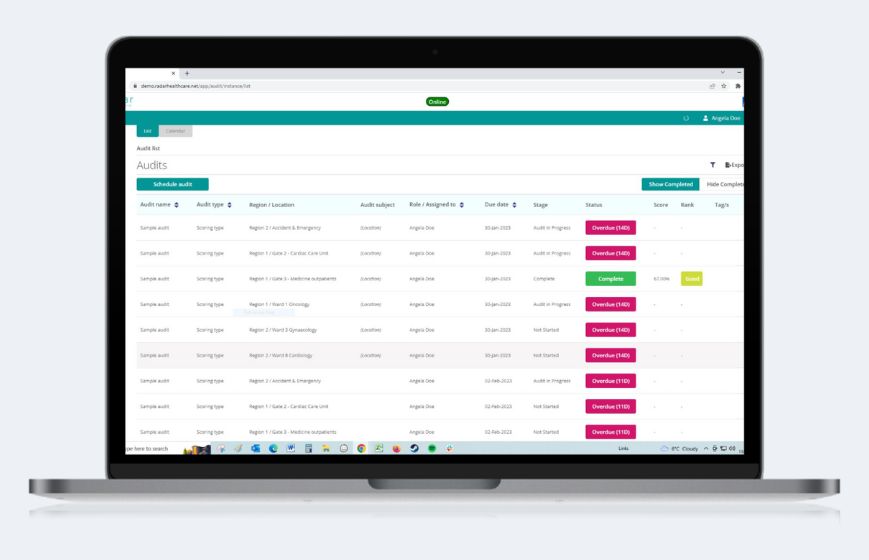
Our intuitive system allows health and social care teams to communicate and collaborate on projects, complete tasks more efficiently, and ingrain a culture of continuous improvement.
Speak to our expert team today to see how we can help you and your team deliver the best quality of care, book a consultation below.