PSIRF Webinar Recap: PSIRF Learning Response Tools
09 February 2023
Tags:
PSIRF Webinar Recap: PSIRF Learning Response Tools & Integrating After Action Reviews to Enhance Learning and Safety
In this PSIRF webinar hosted in partnership with HSJ, we delved into the transformative power of the Patient Safety Incident Response Framework (PSIRF) and how integrating After Action Reviews (AARs) can significantly enhance learning and safety within healthcare organisations. Here’s a comprehensive recap of the key points discussed.
Understanding PSIRF
The Patient Safety Incident Response Framework (PSIRF) is a strategic approach designed to improve patient safety by enhancing the way healthcare organisations respond to incidents. PSIRF aims to foster a culture of safety, improve systems and processes, engage and empower staff, and promote continuous learning and improvement.
Key Takeaways from the PSIRF Webinar
1. The Importance of a Learning Culture
A fundamental aspect of PSIRF is creating a culture that prioritizes safety and encourages continuous learning. This involves transparent reporting, open communication, and a commitment to understanding and addressing the root causes of incidents.
2. Integrating After Action Reviews (AARs)
After Action Reviews are a critical tool for learning from incidents. They involve a structured discussion to review what happened, why it happened, and how similar incidents can be prevented in the future. AARs help teams to systematically analyze incidents and develop actionable insights for improvement.
3. Leveraging Technology for Incident Management
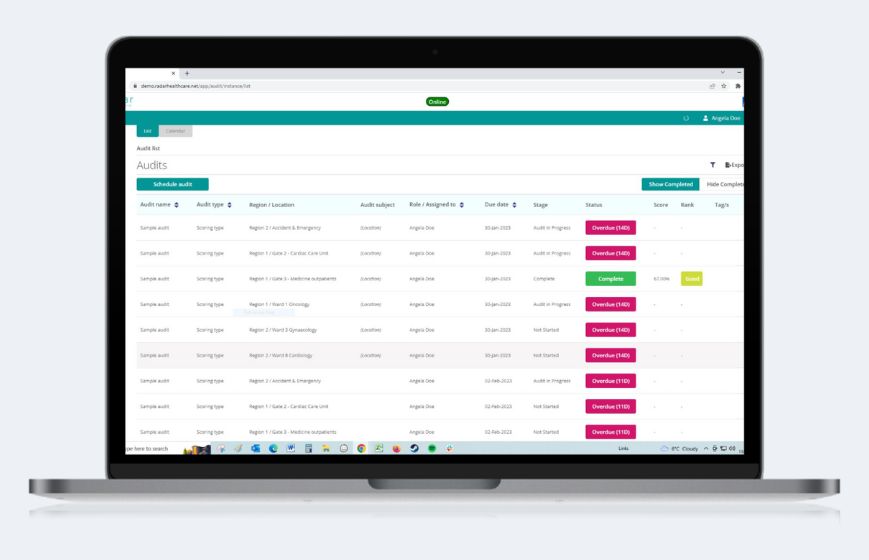
Utilizing advanced technology like Radar Healthcare’s platform can streamline the incident reporting and management process. Our tools offer real-time data access, automated workflows, and powerful analytics to support effective incident response and continuous improvement.
4. Comprehensive Incident Management
Efficiently report, track, and manage patient safety events from initial occurrence through to resolution. Ensure no detail is overlooked and all incidents are addressed promptly.
5. Advanced Analytics for Better Decision Making
Harness AI-driven analytics to identify patterns, uncover insights, and drive continuous improvements in patient safety. This data-driven approach enables healthcare organizations to make informed decisions based on comprehensive analysis.
6. Customisable Dashboards and Reports
Create personalised dashboards to monitor key performance indicators and generate detailed, customizable reports. These tools help healthcare organizations meet regulatory requirements and provide valuable insights into patient safety performance.
Benefits of Using Radar Healthcare for PSIRF
🔧 Customisable Integration: Tailor the PSIRF system to fit your specific needs and existing workflows.
🖥️ User-Friendly Interface: Promote widespread adoption and accurate data entry with an intuitive design.
📊 Advanced Analytics: Drive continuous improvements in patient safety with AI-driven insights.
✅ Comprehensive Incident Management: Ensure all incidents are reported, tracked, and resolved efficiently.
📄 Automated Reporting: Generate detailed reports with ease to meet regulatory requirements and improve transparency.
⏱️ Real-Time Data: Access up-to-date information anytime, anywhere, for timely decision-making.

Summary
Integrating PSIRF with After Action Reviews and leveraging advanced tools like Radar Healthcare can significantly enhance patient safety and organizational learning. By fostering a culture of safety, improving systems, and empowering staff, healthcare organizations can ensure a proactive approach to incident management and continuous improvement.
For more detailed information on how Radar Healthcare can support your PSIRF implementation, contact us today or check out the full webinar at the top of the page.