Technology for continuous improvement
11 June 2019
The CQC’s ‘Celebrating Good Care, Championing Outstanding Care’ report (2017) outlines that technology is influencing the way health and care services are delivered, and that future focus of the CQC will be placed on identifying where providers are successfully harnessing new technology to improve outcomes for people.
This blog post explores quality and compliance trends within health and social care and how technology can help to deliver consistency and embed a culture of good practice in your healthcare organisation.
Common trends
We start by looking at standards of care as there are a series of common trends which demonstrate an increasing requirement for a more joined-up way of monitoring care services and evidencing improvement.
When reviewing data from recent CQC inspections*
- Only 3% of care providers achieved Outstanding
- 64% achieved Good
- 29% Require Improvement
- 4% were deemed Inadequate
In its 2017-2018 ‘State of Care’ report, the Care Quality Commission identified the main areas that contributed to variation in quality were;
- Access to good care and support varies depending on where you live – more consistency is required.
- Quality of care can be improved by good leadership and governance.
- Capacity to meet high demand for care which continues to rise.
- People’s care experiences are determined by how well different parts of local systems work together.
Extracts from CQC inspections also highlight the importance of a structured framework for employee compliance, training and personal development. Onboarding competent and trained staff and the ability to maintain and develop their skill set to deliver effective levels should be a priority for all care services.
“Patient outcomes were hard to identify as little or no reference was made to audits or quality improvements and there was no evidence that the practice was comparing its performance to others; either locally or nationally. Clinical audits did not demonstrate quality improvement.”
“There was no formal staff induction programme in place and there were training gaps in supporting them to develop their skills and knowledge.”
“Recruitment practices were not robust and there were gaps in staff employment checks”
“The practice had a number of policies and procedures to govern activity but some of these were not accessible to staff when needed.”
These issues are often as a result of providers and leaders failing to check the quality of their care, seeking the views of people using the service, administering medicines safely, and making sure that staffing levels are adequate to provide care in a person-centred way.
This highlights how essential it is to have a systematic way to managing quality, ensuring there is a holistic approach to service improvement throughout your healthcare organisation. All too often, there is a disjointed or manual approach to monitoring quality and compliance within health and social care which can:
- Distract from the core focus of the organisation
- Deliver inconsistent results with a high risk of human error
- Be expensive
- Be cumbersome
- Limit scalability for your organisation
But with health and social care in the UK facing unprecedented financial and operational pressures and demands on an already stretched healthcare system, how can care providers deliver better levels of care and evidence quality management and service level improvement to relevant regulatory bodies?
Digital transformation to improve quality and compliance
As technology develops and becomes more affordable, it is no surprise to see a growth in the quality and compliance software market for the health and social care sector. And there is no shortage of evidence to demonstrate the health technology benefits for providers when technology is used effectively to support the delivery of care.
Healthcare organisations are therefore embarking on digital transformation projects to:
- Realise sustainable cost savings
- Increase productivity
- Improve data integrity
- Facilitate sharing of information between systems, organisations and people
- Keep confidential information more secure
- Support environmental policies
Common challenges to a digital approach
If we take a look at common challenges to the introduction of software in a healthcare organisation, the potential benefits to both the providers and the recipients of care often outweigh the concerns.
Cost – The business case for digital adoption is a simple one to write. Whilst there is an upfront investment for the implementation of quality and compliance software – both from a monetary and time point of view – it can without a doubt enable more cost-effective service delivery long-term as it creates efficiencies within the care system.
Digital resilience – The successful integration of any new technology into the workplace requires a highly engaged and appropriately trained workforce. It is therefore essential that digital literacy is a priority and the necessary training given to support the introduction of new software and systems. But this will only work if the software that is introduced is intuitive, has a well-designed user interface and has been developed with users in mind.
Organisational resistance to change – The known barriers to embracing technological changes in healthcare are exacerbated by the precedent of poor previous experience and when paired with lack of trust and fear of the pace of change, engagement can be difficult. Ensuring you take your team on the journey of introducing the system.
Software replacing people – People are what makes the UK’s health and social care system the best in the world. Rather than software ‘replacing’ people, it should support them to offer the most valuable commodity to this sector – time.
* Stats taken from cqc.org.uk latest inspections September 2018.
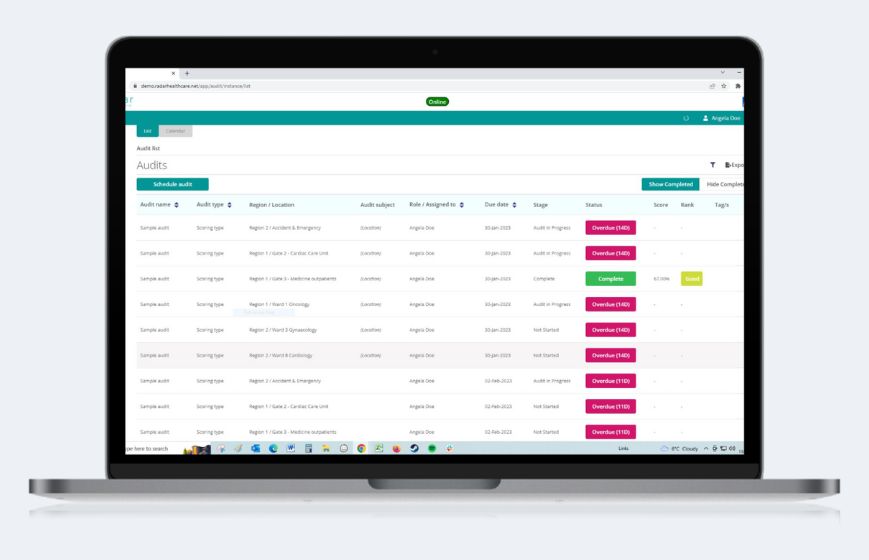
Radar Healthcare
Quality and compliance focused software that helps improve the delivery of health and social care, whilst helping you evidence effectiveness and continuous improvement. We know you aspire to be outstanding, so we help simplify the regulatory complexities you face, giving you more time to focus on delivering excellent care. Want to know more? Get in touch with us today, or book a demo of our software here.