Secondary Care
Free Whitepaper: Incident Reporting in Secondary Care
Download your Free Whitepaper: Incident Reporting in Secondary Care
The NHS has prioritised patient safety incident reporting for many years. Its own 2019 Patient Safety Strategy tells us that by focusing on Insight, Involvement, and Improvement, almost 1,000 extra lives could be saved along with a reduction of £100 million in care costs each year from 2023/24. But in secondary care, reality has not yet matched its ambition.
For a snapshot of where we are today, we commissioned research into incident reporting by hospital ward nursing staff.

The results show the NHS reporting culture has made great strides, with nurses taking reporting seriously and most believing that their reports do lead to better safety outcomes. But our research also found that there is still much work to do, e.g., making it easier to report and to show nurses that their reports are taken seriously.
With the introduction of the Patient Safety Incident Response Framework (PSIRF) and the recent appointment of Henrietta Hughes OBE as Patient Safety Commissioner, we can look forward to a more focused approach to improving healthcare outcomes.
This also shows that there is a 100% commitment and desire from the government, care teams and NHS management to drive quality improvement. The incident reporting culture is healthy. Now we need to give them the data-driven tools to deliver real change.
Staff engagement involves much more than merely giving people the means to be able to report something, good or bad. If they get feedback on what they report and understand the lessons learned, they truly get a sense that you are taking it seriously and are taking action, and that will drive positive change.
How can Radar Healthcare help you?
At Radar Healthcare, we believe in making a difference. We were the first supplier to pass LFPSE testing with NHS Improvement and partnered with Milton Keynes University Hospital NHS Foundation Trust as the first to integrate the system.
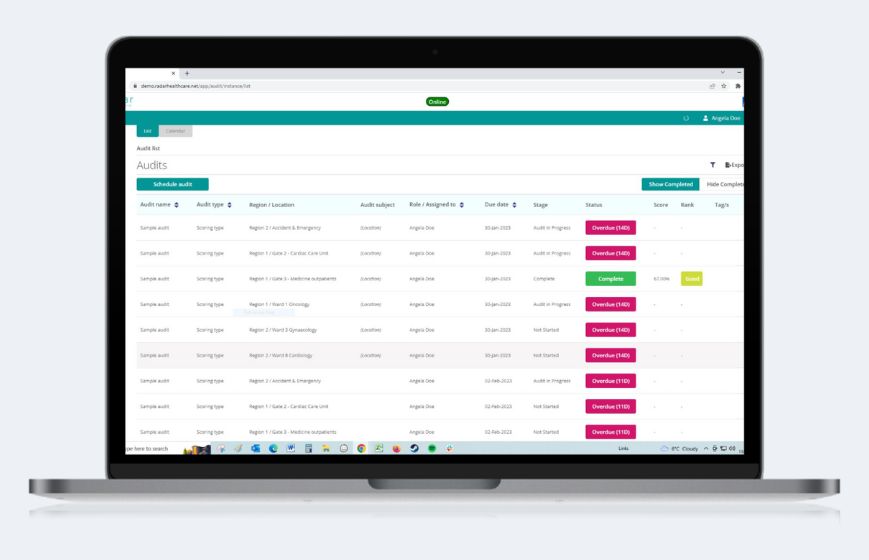
Our award-winning risk, quality, and compliance software is here to help you deliver better healthcare outcomes from day one. Our main aim is to improve patient outcomes and safety, creating a safer experience for all patients. We understand the day-to-day pressures and challenges faced, which is why we are constantly evolving our software to stay on top of the latest requirements.
Find out how Radar Healthcare works with our partners, in NHS and Care as well as specialist services, to provide tailored software for all occasions.
Book a free demo