HSJ Patient Safety Congress 2024: A Focus on People, Tech, and Safety Culture
Tags:
Radar Healthcare at the HSJ Patient Safety Congress 2024
As the headline sponsor of this year’s Health Service Journal (HSJ) Patient Safety Congress, we at Radar Healthcare were thrilled to be a part of so many insightful discussions and powerful sessions.
From exhibiting to hosting private events and leading sessions, we were immersed in key themes that shaped the two days: the importance of feedback, protecting staff wellbeing, harnessing technology the right way, and creating a safe environment for open communication. At the core of these conversations was a shared belief that people are the most valuable resource in healthcare, and their voices must be amplified for lasting improvement.
Here’s a recap of the two day’s events, speaker sessions, and key takeaways…

Session: Creating Safety Every Day in a Degraded System
This keynote session addressed the realities of working within a strained healthcare system. Dr. Aidan Fowler (NHS England), Rob Webster CBE (NHS West Yorkshire ICB), Professor Jane O’Hara (THIS Institute (The Healthcare Improvement Studies Institute)), Dawn Benson (Clinical Human Factors Group), and Andrew Murphy-Pittock (Health Services Safety Investigations Body (HSSIB)) led a conversation around how to maintain safety in an overstretched system.
Key points included:
🧑⚕️ Invest in people: Nurturing and supporting staff are essential for retaining talent and freeing up time for care.
🛠️ Operational readiness: Small, incremental changes can have a positive ripple effect across the healthcare system.
🎯 Tangible actions: Courageously involve staff and patients in decision-making and prioritise constant enquiry over feeling overly assured about safety. Safety is dynamic, requiring continuous evaluation.
🌟 Positive recognition: While challenges persist, there’s still a great deal of good happening in healthcare. Leaders should balance honest conversations about the difficulties with recognition of the positive work taking place daily.
Our Takeaway: Safety culture is not driven by individuals but by the systems they work in. To truly improve, healthcare systems need to change, starting with actively listening to staff and patients, fostering humility, and creating space for honest dialogue.

Session: How AI and Emerging Tech Can Support Early Intervention, Rapid Learning, and Quality Improvement
In this session, Lauren Morgan (Morgan Human Systems), Timothy Bonnici (UCLH), and David Wong (University of Leeds) tackled the integration of AI into healthcare and how it can improve safety and care delivery.
Key insights included:
🤖 AI should be seamless: The most effective AI operates behind the scenes, smoothing out smaller, routine tasks to allow clinicians to focus on patient care.
💡 AI should not be feared but embraced: The panel highlighted how AI is embedded into our everyday (even if you don’t realise it) and should be embraced as a tool to better support productivity and understanding.
📚 Consider training protocols: Like all tech, AI needs to be understood by your workforce to ensure that it is being used safely and correctly.
👥 Think of AI as a team member: Tim Bonnici likened AI to a junior team member with great potential but requiring oversight and guidance. It’s crucial not to follow AI blindly but to use it as a tool alongside clinical judgment.
🤝 Collaboration: Success with AI requires strong collaboration between clinicians and technologists to ensure it addresses real-world healthcare challenges effectively.
Our Takeaway: AI has enormous potential, but it must be implemented carefully, with proper regulation and collaboration to maximise safety and minimise data bias and other risks.

Chief Nurse Lunch: Strengthening Continuous Improvement in Patient Safety Culture
Radar Healthcare hosted an interactive lunch with key nursing leaders to explore how feedback from various stakeholders can improve workplace culture and patient safety.
Paul Johnson (Co-Founder and CEO), Ravi Sehdeva (BDM), and Rhian Bulmer (CPO) led discussions on the importance of sentiment feedback and continuous improvement.
Our Takeaway: Collecting and analysing feedback in real-time from both staff and patients is essential for building a culture of continuous improvement. Involving frontline workers and patients in shaping safety strategies is critical for success.

Session: Positive Family Engagement = Safer Care
In this emotional and thought-provoking session, Rosi Reed and Trevor Stevens from Making Families Count shared their personal experiences and insights on the importance of engaging families in patient care.
👨👩👦 Families as experts: Patients’ families often understand their loved ones better than anyone else. Their insights are invaluable in preventing harm and ensuring safe care.
🚪 Breaking down barriers: Reed and Stevens highlighted the need to create an open, approachable environment where families feel comfortable sharing their concerns without fear of being labeled as “difficult.”
🗣️ Collaborative conversations: MFC provides training to help healthcare professionals engage positively with families during care, emphasising collaboration rather than seeing families as obstacles.
Our Takeaway: Engaging families in patient care not only improves safety but also builds trust and transparency between healthcare providers and those they serve.
Learn more about how to empower families and professionals in our What the HealthTech? Episode featuring Rosi Reed.
Session: Emergency Care – Managing Crowding Pressures and Flow: Risk and Safety
Jono Broad (NHS England South West) and Ian Higginson (Royal College of Emergency Medicine) led a session that addressed one of the most critical challenges facing emergency care: overcrowding and its impact on both clinical outcomes and the quality of human care. They highlighted the dual negatives of this issue, as overcrowding not only compromises patient safety but also significantly affects the wellbeing of healthcare professionals.
- 2/3 of emergency doctors are experiencing significant symptoms of burnout, a direct result of the intense pressures in emergency departments.
- Since 2020, 12-hour stays in emergency departments have drastically increased. Research shows that 1 in 72 patients will die if they remain in emergency care for 8-12 hours.
- Last year alone, 14,000 deaths in England were associated with long waits in emergency departments, underscoring the urgent need for change.
The speakers posed a crucial question: What can be done to stop this?
Our Takeaways:
- Overcrowding affects not just clinical outcomes but also the mental health and resilience of emergency department staff, leading to high burnout rates.
- Prolonged stays in emergency departments dramatically increase mortality risk, making timely patient flow a life-or-death matter.
- The session emphasised the need for system-wide interventions that prioritise both patient safety and staff wellbeing. Reducing wait times, increasing capacity, and implementing more efficient care pathways were highlighted as critical measures to address these challenges.
Session: Reframing incident reporting as a positive
One of the standout sessions of the day was led by Charles Vincent (Oxford University), where the focus shifted to reframing incident reporting as a positive, proactive practice in healthcare. This session highlighted the role that modernised technology can play in fostering a system-level responsive culture – one that is not reactive, but preemptive in addressing issues.
The session discussed the importance of evolving towards a restorative, compassionate, and just culture that benefits staff, patients, and families alike. By shifting the mindset around incident reporting from blame to learning, healthcare systems can create an environment where openness and collaboration thrive.
The session also stressed the critical role of group and multidisciplinary learning in driving improvement. Ensuring that all stakeholders, including staff, patients, and families, are involved in this learning process can lead to more comprehensive solutions and safer care environments.
Session: The Importance of Speaking Up and How Technology Can Strengthen Continuous Improvement in Patient Safety Culture
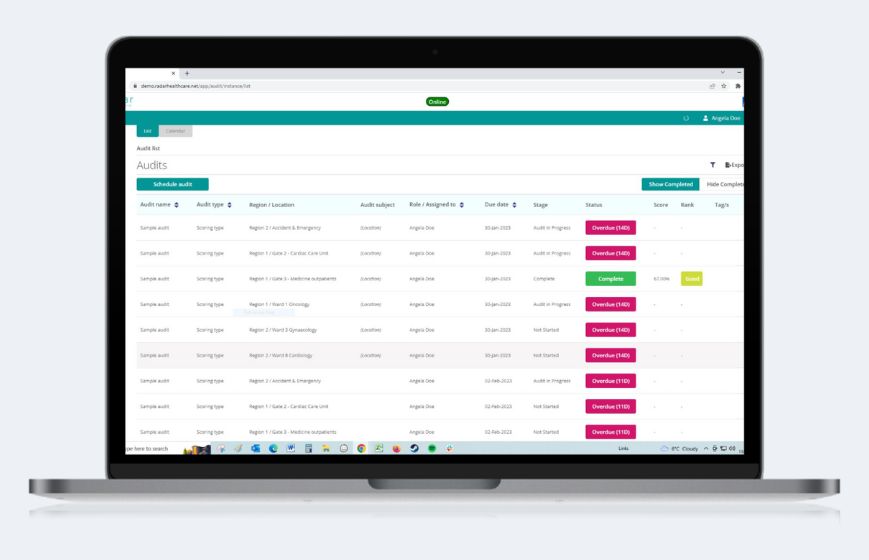
The session, hosted by Rhian Bulmer, CPO at Radar Healthcare, explored how integrating people, processes, and technology can enhance patient safety culture. This discussion emphasised the critical role of speaking up in healthcare environments and demonstrates how Radar Healthcare’s system supports continuous improvement through innovative features.
📝 Better and Balanced Reporting: Reporting of errors, near misses, and unsafe conditions are crucial for identifying and addressing potential risks before they result in harm. Learn how to create a safe and accurate reporting culture.
🌱 Cultural Change: Fostering a culture of transparency and trust where staff feel empowered to speak up without fear of retribution.
📊 Continuous Improvement: How to use data and insights to drive quality initiatives and policy changes.
📋 Standardised Reporting: Implementing clear, consistent procedures for reporting and responding to safety incidents.
🔗 Integrated Systems: Combining electronic patient records with risk and compliance data to provide a holistic view of patient safety.
⚙️ Automated Solutions: Utilising technology to automatically identify areas for improvement and implement changes, reducing the burden on staff and enhancing efficiency.
🏛️ Alignment with National Policy: Using data to proactively identify and address areas of concern, staying ahead of regulatory requirements.
The session underscored the importance of a robust patient safety culture supported by technology. By promoting a culture where speaking up is encouraged and valued, and leveraging advanced tools like Radar Healthcare’s risk, quality and compliance system, healthcare organisations can achieve continuous improvement, ensuring better outcomes for patients and a safer working environment for staff.

And that’s a wrap for 2024!
As always, the Patient Safety Congress was packed with actionable insights and powerful discussions. From leveraging tech to improve patient safety to fostering a culture of feedback, one message was clear: people are the heart of healthcare. As we look to the future, creating safer, more transparent, and patient-centered care will require continuous collaboration between healthcare providers, tech innovators, and patients themselves.
A big thank you to all the speakers, attendees, and our partners at HSJ for making the event such a success. We look forward to next year!