ICSs: all about provider collaboratives
Tags:
 In our blog series on Integrated Care Systems (ICSs), we cover what they are, their structure, benefits and how technology plays a significant role. In this blog, we deep dive into the partnership and delivery structure of an ICS, particularly provider collaboratives. We cover the benefits of these collaborative arrangements on health and care services in England.
In our blog series on Integrated Care Systems (ICSs), we cover what they are, their structure, benefits and how technology plays a significant role. In this blog, we deep dive into the partnership and delivery structure of an ICS, particularly provider collaboratives. We cover the benefits of these collaborative arrangements on health and care services in England.
What are provider collaboratives?
Involving at least 2 NHS trusts, provider collaboratives are partnership arrangements spanning several places, with the aim of effective decision making. They cover the geographical footprint of a system, which is 1-2 million people. Their purpose is to decrease inequality in health outcomes, service access, and experience. They should improve resilience and provide mutual aid, and ensure specialisation and consolidation occur where this improves outcomes and value.
Organisations within this partnership working are NHS trusts, VCSE (voluntary, community and social enterprise) organisations and the independent sector.
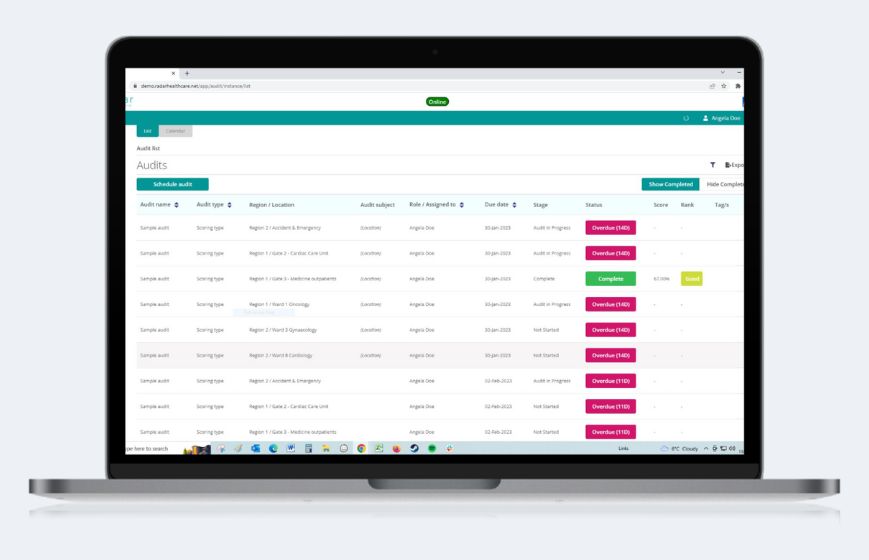
Radar Healthcare supports every area of ICSs
What are the benefits of provider collaboratives?
Benefits at scale and mutual aid have already been proven in some already established provider collaboratives.
For example, NHS-Led Mental Health, Learning Disabilities and Autism (MHLDA) provider collaboratives are groups specialising in mental health. They work with families and communities to design and deliver specialised services across a wide area. The lead NHS provider subcontracts with other providers, including members of the collaborative, to deliver services.
Over 2 years, a pilot over 15 sites led to more than 70% fewer admissions to CAMHS units (Child and adolescent mental health services), as well as savings of over £30 million which can be invested in new services.
From examples like this and others, the benefits of scale that can be delivered include:
Reducing unwarranted variation in outcomes
New evidence-based models of care developed by the collaborative working of partners can reduce unnecessary variation in care. If staff all use the same processes and procedures, they can move between sites easier and work more efficiently.
Technology is the key to standardising processes
Reductions in health inequalities
Over the entire care pathway, provider collaboratives can instil joint accountability, and ensure the timeliness and access to health services is equal for all.
Greater resilience across systems, including mutual aid and reducing workforce pressures
Members support each other to improve health and social care, with strong leadership teams helping others, especially when it comes to complicated changes. Working as a large team, staff can flexibly work across different sites where their contracts, cultures and processes are aligned. As a result, patient experience should be improved with more seamless working of staff, and any demand changes in particular locations can be responded to with the help of others.
Better recruitment, retention and development of staff
Smaller providers can struggle with recruitment and retention, so if they work together with larger ones, there will be a big pool of staff where leaders can be easier developed. Shared programmes can be invested in to improve access to staff training.
Consolidation of smaller or specialised services
Outcomes for patients can be improved if providers agree on how and where to consolidate specialised services.
Efficiencies and economies of scale
Joining up some support and services, or procurement for purchasing power can save members money.
The difference between provider collaboratives and place-based partnerships
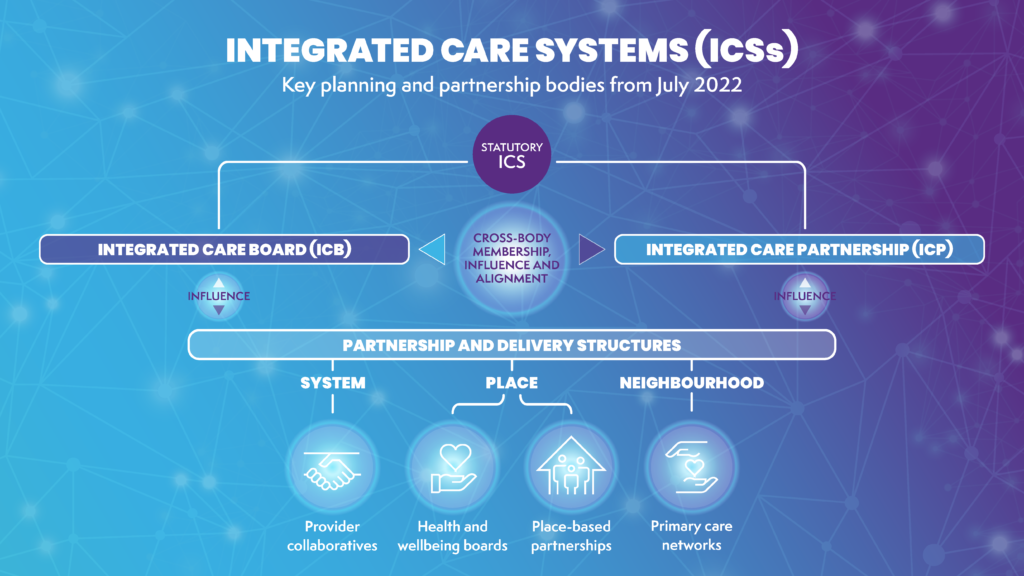
Place-based partnerships cover a smaller geographical footprint than provider collaboratives, called Places, with a population of 250-500,000. They can include ICB (integrated care board) members, local authorities, VCSE organisations, NHS trusts, Healthwatch and primary care.
Place-based partnerships will work with provider collaboratives. NHS providers who are members of a provider collaborative will be involved in a place-based partnership in the place/s it is geographically based.
Provider collaboratives and place-based partnerships may work together on understanding population health indicators in local areas and using patient feedback collected at place and neighbourhood levels across different providers. Providers working across both collaboratives and place-based partnerships will be able to build joint engagement programmes, avoid duplication and help ensure alignment with ICS priorities.
The role of technology in provider collaboratives
A primary aim of provider collaboratives is to have standardised processes and procedures for staff so that they are able to support other locations if and when needed. The best way to do this is to introduce software which enforces set processes that the workforce must follow, such as how to report incidents, how to manage risk, and how to analyse and use data.
Radar Healthcare is already equipped for all areas of ICSs, including provider collaboratives. It acts as one central system for all processes and procedures around quality, compliance and risk. As well as having oversight of your full ICS, you can drill down to information on each area and ensure that there is shared learning between those that are performing well to those that may be struggling.